By Goya Dmytryshchak
A leading doctor says GPs are not equipped to deal with a potential outbreak of coronavirus and is calling for “sentinel practices” to be established.
It comes as Australia on Sunday had its first death among at least 29 confirmed cases of COVID-19, with more than 60 countries impacted and a new travel ban imposed on foreign nationals travelling from Iran to Australia.
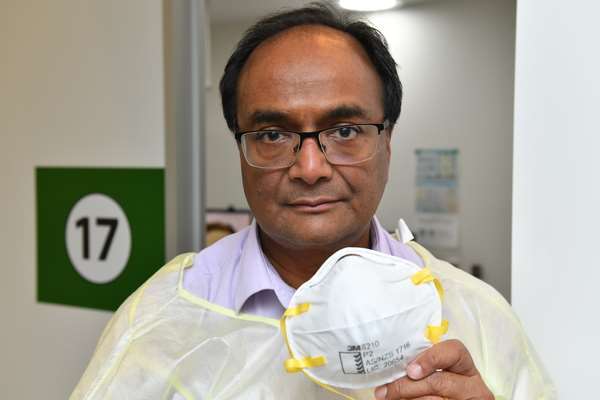
Altona North GP Mukesh Haikerwal said aside from some masks from the federal government, doctors had received little support for dealing with patients presenting with symptoms of the disease.
“We’re not going to face the bullet without a bulletproof vest,” said the former Australian Medical Association president and World Medical Association council chair.
“We feel quite unsupported in general practice land.
“Everybody is telling us to receive patients, screen patients from Bali and so on, but there’s been precious-little support in terms of maybe a few masks come in from federal and nothing really from state.
“No advice about what to do if we received a case and about cleaning the practice up after the case has been through – and you’ve got to keep the room empty – and a lack of understanding that if you shut down a couple of rooms you can decimate a practice.
“I’d probably end up sending people to casualty rather than keeping them in your practice because you couldn’t afford not to run your practice.”
A worker at a major Melbourne hospital said a lot of GPs did not want to take in suspected coronavirus patients and told patients to go to the emergency department, while the hospital was directing people to call the dedicated hotline on 1800 675 398.
Dr Haikerwal said clear messaging and material support for doctors was needed.
“We want more concerted action so that we are not just saying nice things but actually are prepared if the worst does happen,” he said.
“At the moment, we’re just hoping that the worst doesn’t happen.
“I think there’s no point just being prepared, we need to be actively working through the scenario that this is upon us.
“It may mean that certain practices are set up as what we call ‘sentinel practices’, that are geared up and prepared with gear and people and training so that they can take the load off the rest of the practices.
“Even in hospitals, you wouldn’t just go to an emergency department in hospital; even in hospitals there need to be sentinel areas like that.”
Hospitals in Melbourne’s west are braced for the potential impact of a COVID-19 pandemic, bringing together a team of staff with experience in infectious disease prevention and management, Western Health executive director Natasha Toohey said.
She said the team had been developing contingency plans for responding to a “pandemic”.
“Western Health has experts on staff who have many decades of expertise in responding to infectious disease outbreaks,” Ms Toohey said.
“They are monitoring directions from the Australian government’s chief medical officer, Victoria’s chief health officer, and liaise frequently with health officials at the state and national level.”
Ms Toohey said Western Health had not treated any confirmed cases at this time, however measures were in place to quickly identify and isolate patients with suspected COVID-19.
“We are planning for how high volumes of patients could be managed and how this would impact other services we provide,” she said.
“This is an evolving situation and we are monitoring and modifying our response.”